About Cancer Clinical Trials
What Is a Cancer Clinical Trial?
A cancer clinical trial is a medical research study in which people take part as volunteers. These research studies help doctors find new ways to treat, prevent, and diagnose cancer. Clinical trials can also help identify approaches to manage symptoms and side effects.
All of today’s cancer treatments were proven by clinical trials before they became widely available. The patients who took part in these trials played a critical role in advancing cancer research and improving patient care. Without them, progress against cancer would not have been possible.
Although cancer treatments have improved and patients are living longer, better-quality lives, there is still a long way to go. Fortunately, clinical trials are often available for many types and stages of cancer—including early-stage disease. And, despite common misconceptions, clinical trial participants receive excellent care. Usually, they get either the best cancer treatment currently known for their cancer, or a new, possibly more effective therapy.
Who Can Participate in a Cancer Clinical Trial?

Every clinical trial has a detailed study plan (called a protocol). The protocol includes guidelines, known as eligibility criteria, for who can and cannot take part. Eligibility criteria describe characteristics that all study participants must share, such as:
- Cancer type
- Age
- Medical history
The protocol also outlines the trial’s purpose, goals, processes, and more.
Are Cancer Clinical Trials Safe?
Participant safety is the top priority in all clinical trials. Because of this, every trial must undergo a thorough review process before it can begin. Several groups are responsible for regulating clinical trials in the United States. In particular, an Institutional Review Board (IRB) composed of experts oversees a clinical trial’s design. They help ensure that it is safe, fair, and well planned. Once the trial begins, the IRB continues to watch for safety concerns and signs that researchers are following the rules.
Other groups that regulate clinical trials in the US are government organizations, like the Food and Drug Administration, and Data and Safety Monitoring Boards. These boards are independent groups of experts who check patient safety and data quality.
Informed Consent
Before anyone can join a clinical trial, they must review the details, possible benefits, and risks. A patient’s doctor or another member of the research staff will take time to review the specifics and answer any questions. The research team will also provide printed information, including a form that the patient must sign to enroll in the study.
This process is known as informed consent and its purpose is to ensure the patient is making an educated decision.
The patient does not need to sign the form immediately and may take some time to consider their options, and if they want to participate. If a patient does decide to enroll in a trial, they may still change their mind and leave at any time.

Types of Cancer Clinical Trials
There are several different types of cancer clinical trials.
Treatment Trials
This is the most common type. Treatment trials study new drugs or combinations of drugs, vaccines, or approaches to surgery or radiation therapy.
Prevention Trials
Prevention trials look for ways to reduce the risk of cancer in healthy people.
Screening Trials
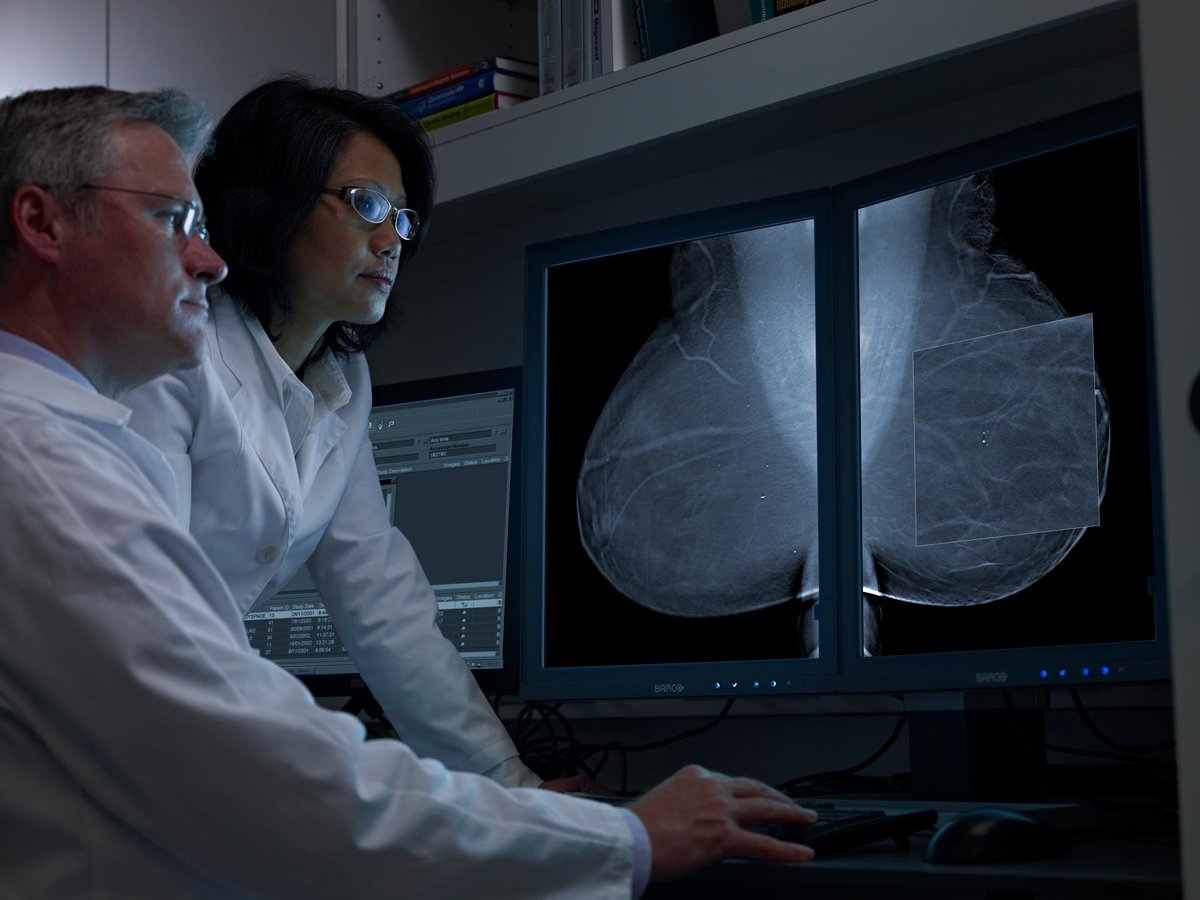
Screening trials explore new methods of finding disease early, when it may be more treatable.
Quality of Life/Supportive Care Trials
These trials aim to improve the quality of life of patients experiencing side effects—short- or long-term—of cancer treatment.
Phases of Cancer Clinical Trials
Cancer clinical trials are usually conducted in a series of steps, called phases. Each clinical trial phase is designed to answer a separate research question. Phase I trials evaluate safety, Phase II trials measure effectiveness, and Phase III trials test against the best existing cancer treatment.
Clinical trial phases are not the same as cancer stages. While cancer stages describe how advanced a patient’s cancer is, clinical trial phases refer to the question or set of questions the trial is designed to address.
Paying for a Cancer Clinical Trial
Federal law requires most health insurance plans to cover routine costs in clinical trials, such as office visits, lab or imaging tests, and standard treatments. These are costs patients would have had for their cancer care whether or not they participated in a trial. Coverage can vary from plan to plan, so patients should always review costs with their health care provider and insurer.
Health insurance plans may not cover research costs, such as the new drug or procedure a clinical trial is testing, or extra lab or imaging tests done specifically for a trial. However, the clinical trial sponsor will often cover these costs. Generally, trials do not cover expenses like transportation to the doctor, parking, or meals.
Finding a Cancer Clinical Trial
New clinical trials are always opening—and they take place at hospitals, cancer centers, and clinics across the US. You do not necessarily need to live in a major metropolitan area to participate in a clinical trial.
View clinical trials led by the Coalition’s member groups. Finally, keep in mind it is always best to speak with your doctor about treatment options, and whether a clinical trial could be right for you.
To search for other clinical trials, try one of these resources.
- Center for Information and Study on Clinical Research Participation (CISCRP)
An organization that provides an online clinical trial search tool and support with searches - ClinicalTrials.gov
A registry of privately and publicly funded clinical trials provided by the National Institutes of Health - EmergingMed Clinical Trial Navigation Service
A platform that provides clinical trial matching, referral, and navigation services free of charge to patients, caregivers, and physicians - Lazarex Cancer Foundation
A foundation that provides assistance finding clinical trials and reimbursing trial-related travel costs